Sarcoidosis is a granulomatous disease of unknown origin. It most commonly affects the lungs, while associated extrapulmonary involvement can be variable. However, pleural involvement, with or without sarcoid pleural effusion, is rare.1,2 Moreover, non-specific systemic symptoms that confound the initial clinical suspicion even further are not uncommon.3 Diagnosis of suspected disease is based on clinical and radiological findings and histological confirmation of non-caseifying epithelioid granulomas. Treatment is still currently based on corticosteroids, which are prescribed on the basis of clinical compromise, progression and/or relapses.1 Disease progression and prognosis are variable.2 As the incidence of this entity is low, we report 1 case of sarcoidosis with PE, and discuss the importance of a differential diagnosis with tuberculous infection.
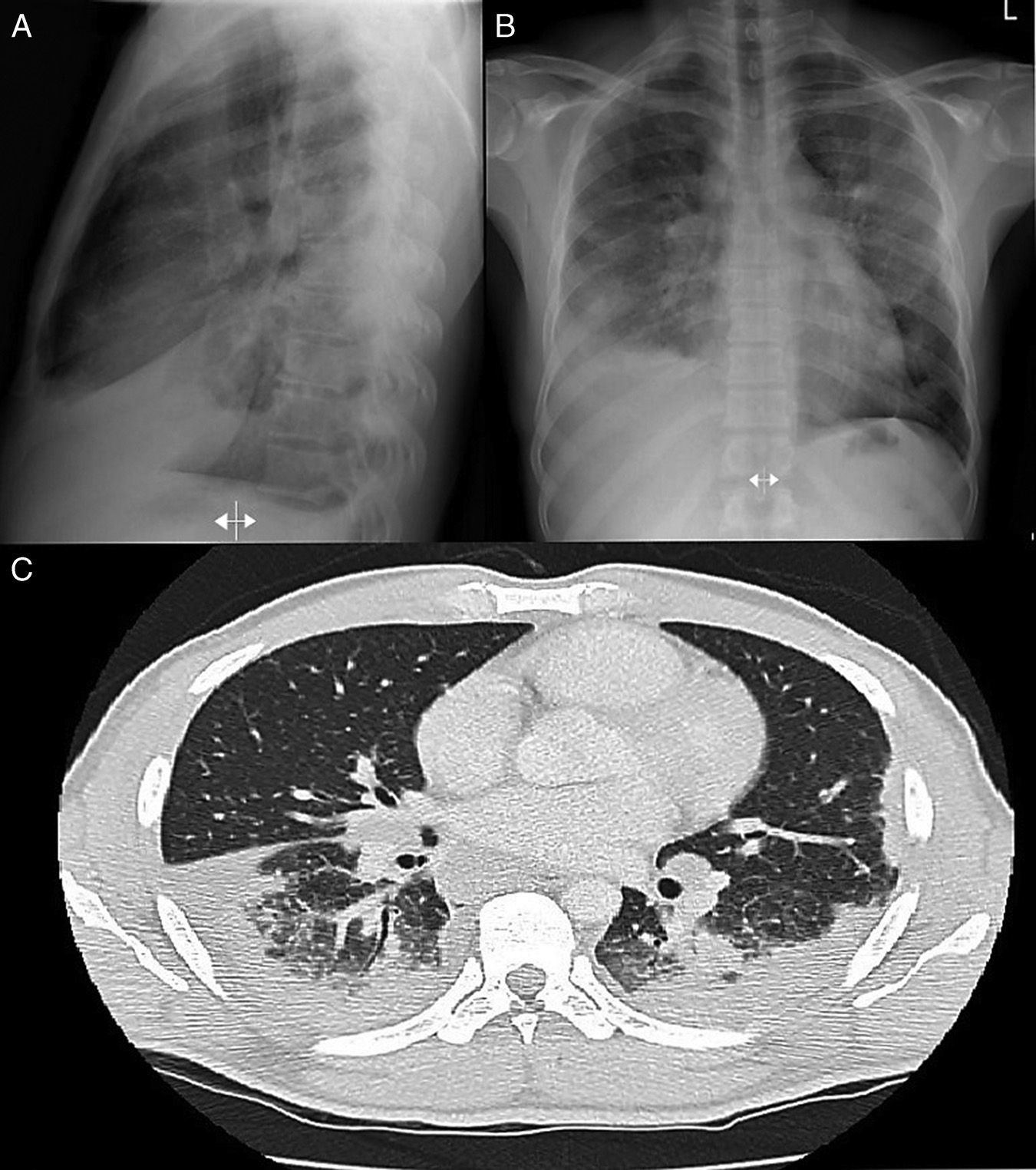
A 38-year-old man, native of Ghana, diagnosed in 2003 with latent tuberculosis (TB), no chemoprophylaxis administered. Episodes of malaria during infancy. He consulted due to a 2-month history of cough, with bloody expectoration, dyspnea, pleuritic chest pain, with weight loss, Afebrile. Of note on physical examination were hypophonesis in the right lung base with crackles and rhonchi up to the middle fields in both sides. Chest radiography revealed bilateral multiple basal alveolar infiltrates with hila of nodular appearance, suggestive of lymphadenopathies, along with right PE (Fig. 1A and B). Of note on clinical laboratory tests: LDH 134, with reduced proteins and albumin, CRP 63mg/dl and ESR 47. Protein electrophoresis spectrum with inflammatory pattern with no monoclonal peak, negative autoimmunity and negative HIV and HCV serologies, previous HBV and HAV. ACE 89.2 (normal<50). Negative for Mantoux booster phenomenon. Serous fluid obtained on thoracocentesis consistent with predominantly lymphocytic exudate, ADA 72. Mycobacteria and fungus-specific staining, cultures and molecular techniques were negative; immunophenotyping showed no clonality but did reveal a significant T cell population with a CD4+/CD8+ ratio of 4/1 (>3.5). After a chest-abdominal PET-CT (Fig. 1C), a bronchoscopy was performed and a transbronchial biopsy obtained, showing necrotizing non-caseifying epithelioid granulomas. Final diagnosis of pulmonary sarcoidosis stage II with secondary PE.
(A) PA chest radiograph. (B) Radiograph of lateral thorax, showing patchy alveolar infiltrates in the left middle and upper lobes. Predominantly right-sided bilateral pleural effusion. Hilar and mediastinal lymphadenopathy of pathological appearance. (C) Axial image of chest CT with intravenous contrast medium showing lymphadenopathy component in the mediastinal, bilateral hilar and periesophageal compartments. Bilateral alveolar involvement predominantly in the subpleural region of both bases, with accumulated nodal lesions and patchy air bronchogram in the subpleural region.
The prevalence of PE in published series of sarcoidosis patients is rare, at between 1% and 2%,3 although some groups have reported rates of up to 8%–10%.4,5 Pleural involvement can appear at any age, but occurs mostly between the ages of 41 and 60 years, with no difference between sexes. It is usually mild-moderate, generally right-sided (48.3%), and occurs in disease stages I and II. It characteristically presents as serous exudate, although 2 distinct types have been described, depending on the etiological pathological mechanism. Lymphocytes are predominant (typically with a CD4+/CD8+ ratio between 2.61 and 8.6).2 Cases described in the literature2 do not state whether patients previously presented a positive PPD, as was the case with our patient, which became negative during the study of the clinical symptoms of sarcoidosis. This effect, known as “immunological paradox”,3 consists of an immune-mediated phenomenon in which, despite intense local inflammation, anergy can develop as a result of dysregulation of the T cells involved in the immunopathology of the disease.
In view of our patient's previous positive PPD and extremely high ADA in PE, active tuberculous infection had to be reliably ruled out, so we performed mycobacteria IGRA, PCR, stains and cultures for 8 weeks in pleural fluid, that were all negative. Sputum smear in bronchial aspirate and urine, and closed pleural biopsy with mycobacterial PCR, cultures and stains were also negative. In view of the high initial suspicion of TB due to the history of untreated latent TB, tuberculostatic treatment was attempted for 10 days while awaiting results, but response was unsatisfactory. The microbiological results, when obtained, were negative, so we strongly suspected pleuropulmonary sarcoidosis in a black patient and began treatment with corticosteroids. Clinical symptoms and laboratory inflammatory parameters improved, and PE resolved, confirming the initially suspected diagnosis.
Finally, given the evidence of previous exposure to TB and current corticosteroid therapy, our patient was given chemoprophylaxis on the assumption that the PPD skin test was a false negative associated with immune system changes due to the disease itself.
Please cite this article as: Fontecha Ortega M, Rodríguez Álvarez SJ, García Satué JL. Derrame pleural: una presentación poco frecuente de sarcoidosis. Arch Bronconeumol. 2017;53:170–171.