Although the Spanish Guidelines for the Management of Asthma (GEMA) include the oral corticosteroid test (OCT) in the diagnosis of asthma with bronchial obstruction and asthma-COPD overlap syndrome (ACOS),1 the most appropriate methodology for performing this test and its clinical utility remain unknown.
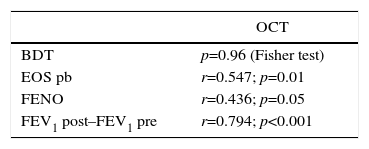
Among asthma patients monitored at the dedicated asthma clinic of the Hospital Lucus Augusti, Lugo, Spain, 122 had bronchial obstruction (BO), despite treatment with a combination of inhaled corticosteroids and a long-acting β-agonist. Twenty-two of them (50% women, 57.51±11.74 years of age) underwent OCT (deflazacort 30mg/3–4 weeks, withdrawal confirmed by electronic prescribing data). A total of 66.7% had non-allergic asthma and 90% had blood eosinophilia (≥ 3%). Mean FEV1 was 52.14% predicted, and 58% had a positive bronchodilator test (BDT). Seventy-seven percent had late-onset eosinophilic asthma, and 36% had smoked >10 pack-years. In total, 27% of patients had complete response (normalization of FEV1) with OCT, 36% had partial response (improvement of FEV1≥200ml compared to previous post-bronchodilator FEV1), and 37% had a non-significant response. An OCT was considered positive when response was at least partial. Of the 10 current or former smokers with eosinophilia, 3 did not respond to the test, suggesting a diagnosis of ACOS. OCT test results were unrelated to the BDT, and showed a weak correlation with FENO values and with the number of eosinophils in peripheral blood (Table 1). FEV1 improved by 487ml and the asthma control test score rose from 17.38 to 21.29 after a follow-up of 32.55 (± 12.67) months and successive therapeutic modifications that did not include oral corticosteroids. A strong correlation was observed between OCT and FEV1 improvement during follow-up (Table 1), but this was not related with BDT results (Student t test; p=0.99).
OCT Results and Other Variables of Interest.
| OCT | |
|---|---|
| BDT | p=0.96 (Fisher test) |
| EOS pb | r=0.547; p=0.01 |
| FENO | r=0.436; p=0.05 |
| FEV1 post–FEV1 pre | r=0.794; p<0.001 |
EOS pb: eosinophils in peripheral blood; BDT: bronchodilator test; FENO: fraction of nitric oxide in exhaled air; FEV1 post–FEV1 pre: difference between FEV1 achieved at the end of follow-up and the initial value; OCT: oral corticosteroid test.
Few studies have been conducted on the effect of a short regimen of corticosteroids in patients with stable, severe asthma: ten Brinke et al.2 found that intramuscular triamcinolone 40mg improved lung function and inflammation within 2 weeks in 22 patients with ≥2% eosinophils in sputum. Dente et al.3 reported similar results with 0.5mg/kg prednisone in 59 patients with severe refractory asthma. However, these studies do not provide information on the nature or prognostic capacity of the OCT.
In short, this preliminary study suggests that the OCT measures a different type of bronchodilation than the BDT, and that responders show improvements in long-term lung function after therapeutic intensification. A prospective study is needed to determine the appropriate dose and length of administration of corticosteroids, and to analyze if the OCT is associated with a specific inflammatory phenotype and if it can predict response to biological treatment.
Please cite this article as: Riaño Pérez A, Pérez de Llano LA, Mengual N, Golpe R. Significado clínico del test con corticoides orales en el asma con obstrucción fija. Arch Bronconeumol. 2017;53:40.