Severe pulmonary emphysema appears in advanced phases of patients with chronic obstructive pulmonary disease (COPD). It is defined as the abnormal and permanent distention of the air spaces distal to the terminal bronchioles and entails a loss of pulmonary elasticity and early closure of the respiratory tract during expiration. All this causes dynamic pulmonary hyperinflation with the consequent air trapping. Despite the optimization of the medical treatment, these patients present a deterioration in lung function and an increase in dyspnoea, so it is necessary to look for therapeutic alternatives such as endoscopic volume reduction (ELVR). In GOLD1 and GesEPOC2 included that after a good selection of patients3–5 (severe emphysema predominant of the upper lobes and lower exercise capacity) the ELVR has demonstrated an improvement in lung function, quality of life and in survival.6–12 This is due to, after the volume reduction, lung volume decreases, which leads to a decrease in static pulmonary hyperinflation and consequently, dynamically, improving lung mechanics and decrease in dyspnoea.13 Despite the improvement in most patients, there is a percentage, which after the treatment, does not present an increase in the quality of life and lung function is similar. In these cases, there is uncertainty in the therapeutic approach. Until now, ELVR options described have been the application of various sessions of thermal vapour14 or even the placement of valves in contralateral bronchi.15 Next, we will describe two cases where we apply one of the possible alternatives which would be the placement of valves and the application of thermal vapour in the same patient.
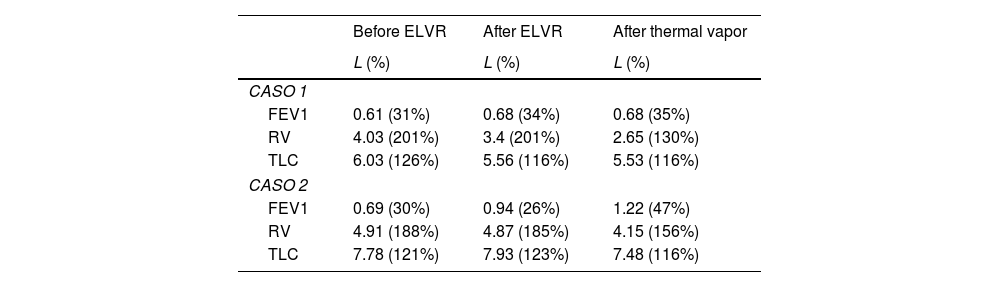
The first case was a woman with severe emphysema and grade III dyspnoea on the mMRC scale with the functional tests described in Table 1. The result of the quantitative study using the specific software StratX® (PulmonX Inc., Redwood City, CA, USA) was that the right upper lobe had a destruction of 73% of the lung parenchyma (<910Hounsfield unit) and a volume of 1292ml, so we decided to treat this lobe. As the major fissure was incomplete, the CHARTIS® system (PulmonX Inc., Redwood City, CA, USA) was performed, which showed its integrity. Two endobronchial valves were placed in segments 2 and 3 of the right upper lobe (segment 1 was absent). Functional testing showed an 11.5% improvement in FEV1 and a reduction in residual volume (RV) and total lung capacity (TLC) of 15.6% (630ml) and 7.8% (470ml), respectively. After a year, the patient presented clinical deterioration, so, after being rejected for transplant, we decided to apply thermal vapour treatment on the anterior segment of the left upper lobe (8.5cal/g). After one month, there was a decrease in dyspnoea (Dyspnoea II mMRC) and improvement in air trapping with a decrease in TLC by 0.5% (30ml) and RV by 22% (750ml).
Functional tests.
| Before ELVR | After ELVR | After thermal vapor | |
|---|---|---|---|
| L (%) | L (%) | L (%) | |
| CASO 1 | |||
| FEV1 | 0.61 (31%) | 0.68 (34%) | 0.68 (35%) |
| RV | 4.03 (201%) | 3.4 (201%) | 2.65 (130%) |
| TLC | 6.03 (126%) | 5.56 (116%) | 5.53 (116%) |
| CASO 2 | |||
| FEV1 | 0.69 (30%) | 0.94 (26%) | 1.22 (47%) |
| RV | 4.91 (188%) | 4.87 (185%) | 4.15 (156%) |
| TLC | 7.78 (121%) | 7.93 (123%) | 7.48 (116%) |
The second case was a man with severe emphysema and grade III dyspnoea on the mMRC scale with the functional tests described in Table 1. According to the quantitative study, we wanted to treat the right upper lobe and the middle lobe (76% density<−910Hounsfield unit and volume 3111ml) but after verifying the presence of collateral ventilation in the CHARTIS® due to the presence of an incomplete major fissure, we decided to treat the left upper lobe (79% density<−910Hounsfield unit and volume 2253ml). Four valves were placed in segments 1+2, 3, 4 and 5 of the left upper lobe. After 14 days the patient present clinical deterioration and was diagnosed with thromboembolic disease (deep vein thrombosis and pulmonary thromboembolism). After the complication, there was initial subjective improvement with subsequent deterioration. FEV1 improved by 36.2% but air trapping was similar with a 0.8% reduction in RV (40ml) and a 1.9% (150ml increase) increase in TLC. Therefore, after one year without improvement, we decided to apply thermal vapour treatment on the apical segment of the right upper lobe with 8.5cal/g. After one month, the patient presented a great subjective improvement in dyspnoea (Dyspnoea I mMRC), increase 29.8% FEV1 and decrease in air trapping (Decrease 450ml TLC and 720ml RV). Neither of the two cases presented complications after the second ELVR.
The use of thermal vapour treatment adjuvant to valve placement in patients without improvement after the first endoscopic volume reduction treatment is a therapeutic option to consider. We have obtained good results without any incidence in these first two cases, but a large study is recommended to verify the effectiveness and possible adverse effects of this technique.
FundingThis study did not receive any type of funding.
Conflict of interestsThe authors state that they have no conflict of interests.