Intercostal pulmonary hernias are relatively unusual, and the most frequent causes are trauma and thoracic surgery. Diagnosis is almost always made by standard X-ray and chest CT scan. However, ambiguous cases can be diagnosed by chest ultrasound.
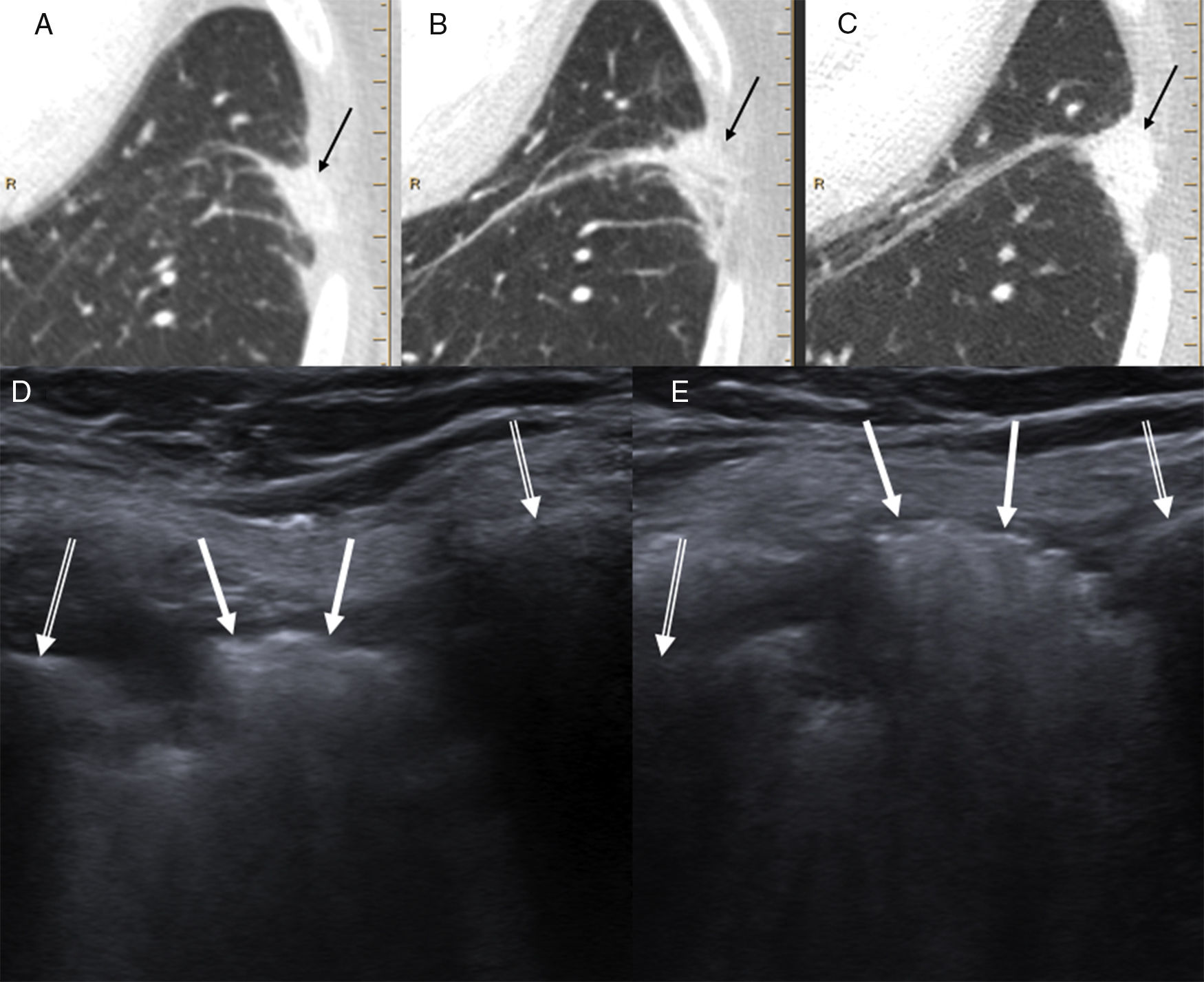
We report the case of a 65-year-old woman with a history of stage IB lung adenocarcinoma who had undergone left upper lobectomy by video-assisted thoracoscopy. The patient reported no pain, and local physical exploration of the surgical wound was normal. In the last follow-up chest CT scan, peripheral pulmonary opacity measuring approximately 24mm in length was visualized, with minor extension to the intercostal space, which had increased in size and density compared to the first postoperative CT scan (Fig. 1). This radiological finding suggested focal pulmonary atelectasis, although local malignant recurrence could not be ruled out. The case was presented to the multidisciplinary thoracic tumor committee of our hospital and the decision was taken to perform ultrasound-guided biopsy. The ultrasound revealed an intercostal pulmonary hernia between the left seventh and eighth ribs, clearly demonstrated by the Valsalva maneuver (Fig. 1), consistent with the peripheral pulmonary opacity seen on CT. The patient remained asymptomatic at all times, so we decided to take a wait-and-see approach.
(A–C) Series of follow-up CTs showing a left laterobasal peripheral pulmonary opacity with minor extension to the intercostal space gradually increasing in size and density (black arrows). (D) Chest ultrasound (Valsalva maneuver) showing a hyperechogenic lesion (white arrows) in the intercostal space between the lateral arches of the left seventh and eighth ribs (double white arrows), which mobilized during respiration. (E) Lesion protruding significantly toward the chest wall during the Valsalva maneuver. The patient was diagnosed with intercostal pulmonary hernia probably associated with thoracoscopy entry port for performing left upper lobectomy
Pulmonary hernias are uncommon protrusions of pleura-covered lung through the chest wall.1–6 Most are thoracic or intercostal hernias (70%–80%).7 Between 78% and 80% of hernias are acquired, and classified as spontaneous, traumatic, or pathological. The underlying mechanism of acquired pulmonary hernias consists of a weakness in the intercostal space enhanced by an increase in intrathoracic pressure, as occurs during coughing or physical effort.2 The chest wall is weaker between the costochondral junction and the sternum and, posteriorly, between the costal angle and the vertebrae.2 Most acquired hernias are caused by trauma, but postsurgical hernias are common, particularly after cardiothoracic surgery by thoracoscopy or minimally invasive techniques.8–12 The site of a thoracoscopy port is not usually sutured,9 so post-procedure pulmonary hernias can appear, as in our case.
On physical examination, pulmonary hernias usually appear as a mass in the chest wall that increases with cough or during the Valsalva maneuver. They can be asymptomatic and detected by chance.3
The initial assessment can be by chest X-ray, although results are usually normal.5 When the hernia is displayed in profile, the border of the lung can be seen beyond the rib cage (“lung beyond the rib” sign). In contrast, when the hernia is seen from the front, a hyperlucent focal area can be detected (“lucent lung” sign).3 X-rays performed during the Valsalva maneuver or in expiration can show an increase in the size of the hernia.2,3
Most cases are diagnosed by CT, when protrusion of the lung through the chest wall is observed. An increase in the intercostal space can be seen, except in the case of hernias associated with prior thoracoscopy.3 The administration of intravenous contrast is useful for visualizing the vascularization of the herniated lung and for excluding strangulation,1–3 and images during expiration or Valsalva maneuver can show occult pulmonary hernias.3
Chest ultrasound can be used for assessing lesions of the lung, chest wall, pleura, diaphragm, and some parts of the mediastinum, in addition to serving as a guide for possible biopsy.1,13 It has advantages over other techniques, including the lack of ionizing radiation, the possibility of performing it at the bedside, assessment in real time, and accessibility.14 Pulmonary hernias present on chest ultrasound as hyperechoic intercostal lesions due to the presence of inflated lung,1 with an absent hyperechogenic pleural line between the 2 ribs of the intercostal space.15 Ultrasound can be useful for pulmonary hernias when CT is not immediately available or if the presentation on this imaging test is atypical. In our case, diagnosis was made by chest ultrasound because when the CT was performed there was no clinical suspicion of intercostal pulmonary hernia, so no expiration or additional Valsalva maneuvers were conducted that could potentially have demonstrated this condition.
Please cite this article as: Porres DV, Pallisa E, Sánchez AL, Persiva O. Utilidad de la ecografía torácica en el diagnóstico de las hernias pulmonares intercostales. Arch Bronconeumol. 2019;55:225–226.