We present the case of a 13-year-old female with febrile neutropenia in the context of medullary aplasia secondary to chemotherapy treatment for acute lymphocytic leukemia. An opportunistic infection was suspected and Galactomannan test was performed with a positive result.
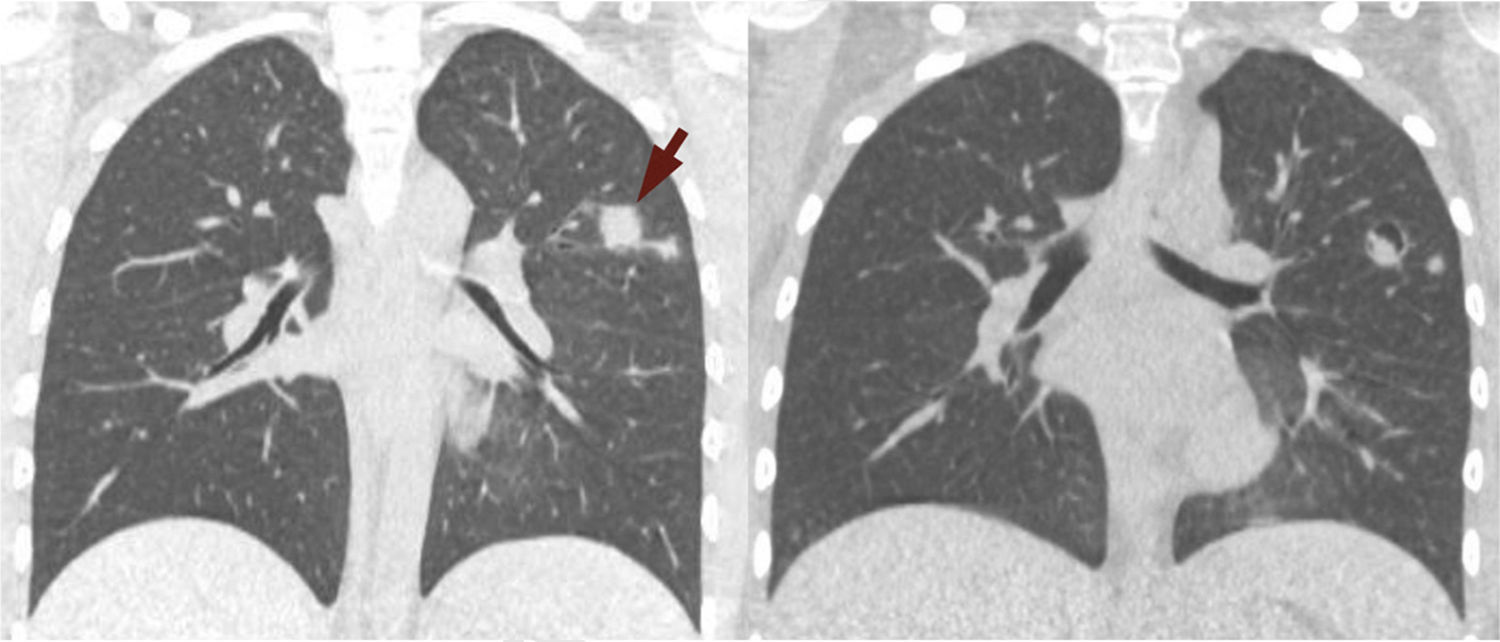
A CT-scan performed to evaluate any possible lung involvement, revealed multiple solid pulmonary nodules with bilateral distribution and upper-lobe predominance. These nodules showed ill-defined margins and exhibited a halo of ground-glass attenuation, or “halo sign” (Fig. 1 – left). In the clinical context, these findings corresponded to hemorrhagic infarcts and were highly suggestive of angioinvasive aspergillosis. Nevertheless, other much less common entities, such as Mucor and Candida, herpes simplex and cytomegalovirus, Wegener granulomatosis, Kaposi sarcoma and hemorrhagic metastases may present with similar findings on CT.1
Antifungal therapy for aspergillosis was administered and the patient made good progress. A follow-up CT performed after 3 weeks of treatment showed cavitation within the nodules, with a small solid component. This is called the “air crescent sign” (Fig. 1 – right), and appears in 50% of the cases.2 When it is seen after the “halo sign”, it reaffirms the diagnosis of aspergillosis and represents the separation of necrotic and healthy parenchyma.1
Please cite this article as: Sánchez VV, García AG, Garmendia FS. Un caso de aspergilosis angioinvasiva. Arch Bronconeumol. 2017;53:273.