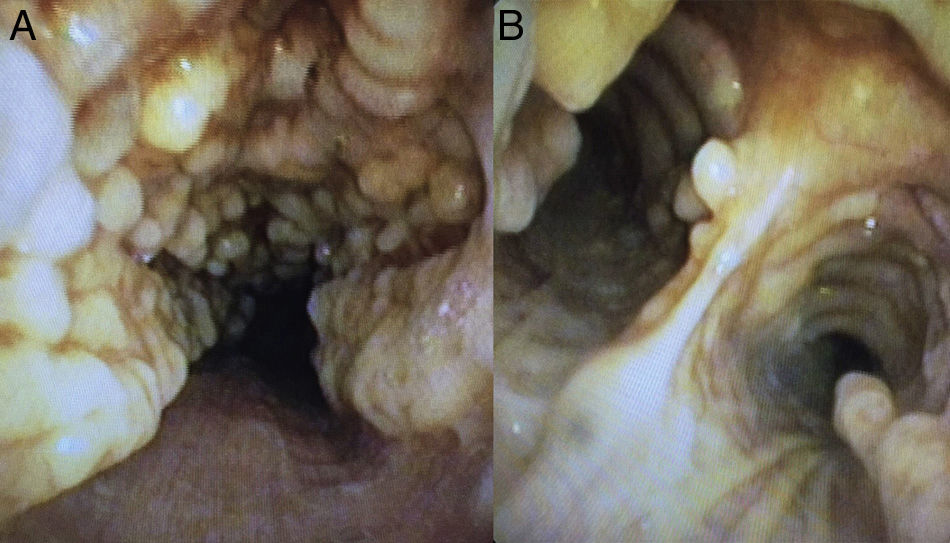
We report the case of a 78-year-old woman with an incidental finding of a pulmonary nodule measuring 18mm in the right upper lobe in a chest computed tomography study performed to determine possible myasthenia gravis. The patient had no respiratory symptoms. A bronchoscopy was performed, revealing significant irregular nodular involvement of the anterolateral wall of the trachea and main bronchi, with a stony consistency, not impinging on the pars membranosa in any way (Fig. 1). Given these characteristic findings, tracheobronchopathia osteochondroplastica was diagnosed.
Tracheobronchopathia osteochondroplastica is a rare benign disease of unknown etiology that affects the trachea and, to a lesser extent, the main bronchi. It is caused by the formation of cartilaginous or bony submucous nodules that project into the lumen of the airway, with no involvement of the posterior wall.2 Visualization of these lesions on bronchoscopy is sufficient to confirm diagnosis, without the need for a histology study.1,2 However, biopsies are performed if bone or calcification of the submucosa is seen. The disease course is benign and slow, and complications are unusual.
Please cite this article as: Sota Yoldi LA, Fernández Mellado R, Vigil Vigil L. Traqueobroncopatía osteocondroplásica, un hallazgo casual. Arch Bronconeumol. 2018;54:280.