Medical graduates’ choice of specialty on leaving the faculty is determined by the results they obtain in their medical internship examinations, and this choice has become an index of both the quality of the university education received and the prestige of the different specialties. Although many factors, exam results in particular, dictate the choice of specialty, one of the most important is degree-level training. However, this is very difficult to assess due to the widely diverging educational programs offered in Spanish universities,1 making it impossible to determine the specific significance of previous training in students’ choice of specialty.
Despite the prevalence of respiratory diseases and the progress made in respiratory medicine, this specialty receives far less attention than it deserves.2 The aim of our study was to assess the impact of practical training in respiratory medicine on the awareness of students and their preferences for the specialty, after they had completed the course entitled “The Respiratory System and the Chest”.
The study involved an anonymous survey conducted before and after a 3-week rotation in the respiratory medicine department, containing 2 items aimed at rating awareness and overall preference for the specialty before and after the rotation on a numerical scale of 1–10 points. Data were uploaded to an Excel spreadsheet and exported to SPSS 22.0, and the relevant tests depending on the variables were applied. The survey was returned by 232 of the 240 students who completed the rotation in the respiratory medicine department between 2015 and 2017. These included 139 women and 93 men with a mean age of 21±1.6 years.
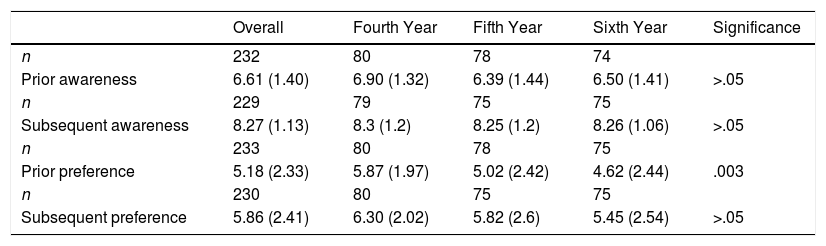
Table 1 lists awareness and preferences before and after the pulmonology rotation. Awareness scored 6.61 before and 8.27 after the rotation. The mean increase in awareness was, at 1.66 points, statistically significant (P<.01). The difference was positive in all courses, with no differences depending on the course in which the rotation was performed (fourth, fifth or sixth-year studies). With regard to preference, the initial score was 5.18 (95% CI 4.8–5.5). Significant differences were observed between courses; these were greater in fourth-year students and lower in sixth-year students. At the end of the rotation, preference scored 5.86, with an increase of 0.68 points (P<.01). The change in preference was positive in all courses, but there were no significant differences between before and after.
Awareness of and Preference for Pulmonology Before and After Rotation.
| Overall | Fourth Year | Fifth Year | Sixth Year | Significance | |
|---|---|---|---|---|---|
| n | 232 | 80 | 78 | 74 | |
| Prior awareness | 6.61 (1.40) | 6.90 (1.32) | 6.39 (1.44) | 6.50 (1.41) | >.05 |
| n | 229 | 79 | 75 | 75 | |
| Subsequent awareness | 8.27 (1.13) | 8.3 (1.2) | 8.25 (1.2) | 8.26 (1.06) | >.05 |
| n | 233 | 80 | 78 | 75 | |
| Prior preference | 5.18 (2.33) | 5.87 (1.97) | 5.02 (2.42) | 4.62 (2.44) | .003 |
| n | 230 | 80 | 75 | 75 | |
| Subsequent preference | 5.86 (2.41) | 6.30 (2.02) | 5.82 (2.6) | 5.45 (2.54) | >.05 |
Two cut-off points of 6 and 8 points in initial awareness were established to assess the influence of prior awareness on preference for the specialty. In both cases, there was a greater increase in preference (P<.01) among students with a lower initial awareness of the specialty.
Theoretical teaching is essential for students to learn about the specialty, but practical clinical training is the cornerstone of medical education.3 This, however, is affected by the characteristics of the departments in which the students do their rotation,4,5 which are organized on the basis of care needs rather than teaching needs, causing significant distortions. While neither theoretical training nor practical experience are absolutely decisive in choosing a specialty,6 they do influence students’ choices, so teaching is an opportunity to improve the position of pulmonology.
It is clear from our study that, despite having completed “The Respiratory System and the Chest” course, students’ awareness of the specialty is limited (6.6 points) and their preference even more so (5.18 points). However, the pulmonology rotation can be used to improve their awareness of the specialty and increase their preference, both in students who have not yet performed rotations in other departments/specialties (fourth-year students) and in those who have already had this experience (fifth and sixth-year students).
As mentioned above when describing the results, variations in awareness of and preference for the specialty are greater in students with less prior awareness of the field, that is to say, students who initially gave a lower score for their preference for pulmonology showed a greater increase in preference for this specialty after increasing their awareness, and the inverse also applies: those with a lower initial preference significantly increased their awareness and preference scores.
Even assuming that many personal, academic, professional, and geographical factors, aside from degree-level training, determine the choice of specialty, it is clear that undergraduate education is one, if not the only, factor we can influence. This is why we believe that improving theoretical training, and in particular practical training, should be an objective for all SEPAR members involved in undergraduate training.
Unfortunately, few pulmonologists are involved in theoretical training; however, a great many are involved in practical training in the hospital setting, and this will give us the chance to improve not only clinical training, but also the perception of the specialty. According to students, there is much room for improvement in practical clinical training,7 so we must seize this as a golden opportunity to demonstrate to students the complete and complex nature of our specialty. We must continue to reflect on the improvements needed in practical training for degree-level students, not only to improve their skills, but also to show them the value of our specialty and thus improve our standing among other specialties.
Please cite this article as: Barrueco Ferrero M, Pérez Rodríguez J, Barrueco-Otero E, Bartol Sánchez M. Utilidad de la formación práctica en el conocimiento y preferencia por la especialidad de Neumología de los estudiantes de grado. Arch Bronconeumol. 2019;55:222–223.