We read with great interest the letter to the editor by Laguna Sanjuanelo et al.,1 who reported the case of a 68-year-old woman presenting a space-occupying lesion in the left pulmonary artery (PA), suggestive of intramural thrombus. She was treated with anticoagulants for 1 year. The diagnosis of a tumor was suggested because follow-up radiologic studies showed progression of the intra-arterial lesion. The final diagnosis was small-cell lung cancer metastasis.
The authors commented on the difficulty of determining the nature of this type of lesion. We would like to highlight the role of imaging techniques as important tools in the differential diagnosis between malignant PA tumors and pulmonary thromboembolism. Patients with PA tumors often present with dyspnea, cough, hemoptysis, and/or chest pain. Because these symptoms can mimic pulmonary emboli, some patients are treated initially with anticoagulation therapy.2
The diagnosis of PA tumor should be considered clinically in the absence of risk factors for pulmonary embolism, such as deep venous thrombosis, and when patients show a lack of response to anticoagulant therapy. Other characteristics, such as rapidly developing symptoms, weight loss, fever, anemia, and high erythrocyte sedimentation rate, may be subtle clues for diagnosis.2–4
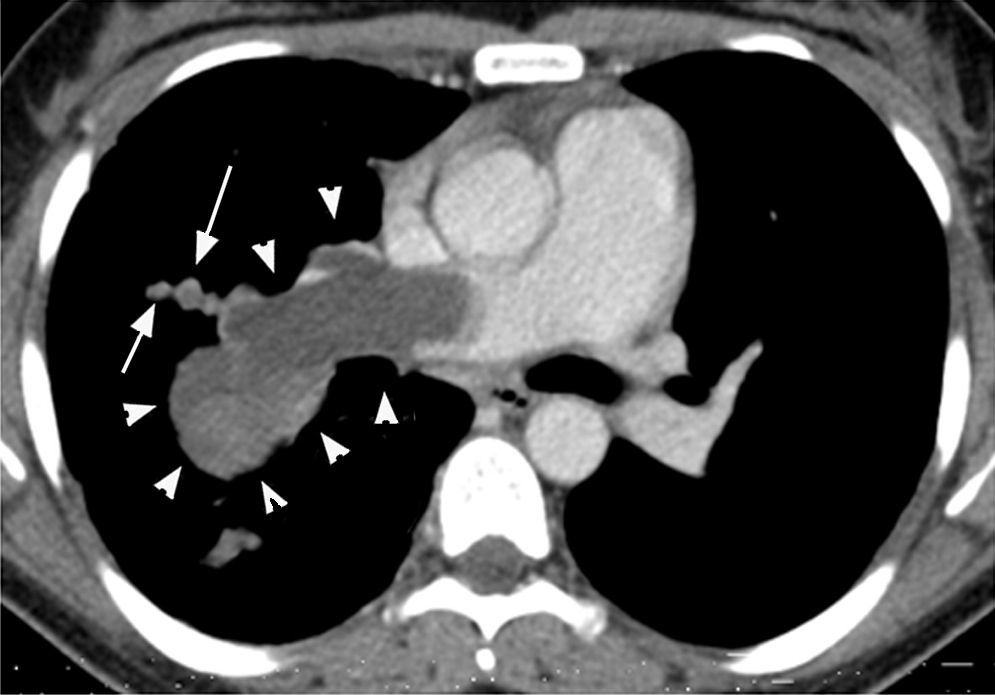
Computed tomography (CT) and magnetic resonance imaging (MRI) are considered to be the most useful tools for differentiation between a tumor and a thrombus.2,3 Both diseases appear as low-attenuation intraluminal filling defects on contrast-enhanced CT, and radiologic differentiation between PA tumor and PA thromboembolism can be difficult.4 CT findings indicative of PA tumor (Fig. 1) include hypodense filling defect with inhomogeneous attenuation occupying the entire lumen of the artery, with an increase in diameter of the involved vessel; contiguous soft tissue-filled PAs with occupation of the entire lumen; vascular distention from tumor growth; beaded peripheral PA; extravascular extension of the thrombus; and patchy and delayed contrast uptake on CT angiography.2,4
Axial contrast-enhanced chest computed tomography of a 35-year-old woman with dyspnea, chest pain, and hemoptysis over several months. An extensive irregular filling defect with inhomogeneous attenuation occupies the right main pulmonary artery and extends into the pulmonary artery branches, with increased vascular diameters (arrowheads). Note also the beaded aspect of a peripheral artery (arrows).
MRI with gadolinium contrast could also help to distinguish a tumor from a thrombus.5 Criteria suggesting PA tumor are similar to those for CT: soft-tissue density in PAs with inhomogeneous high or low attenuation (hemorrhage, necrosis); vascular distension; and heterogeneous uptake after administration of gadolinium, indicating neovascularization.2,3
Early diagnosis and radical surgical resection present the only opportunity for a potential cure.3 A precise preoperative diagnosis enables selection of the best surgical approach and technique, and allows time for ordering prostheses or homografts, which are not always readily available.5 In the presence of suspicious imaging findings, CT-guided needle biopsy may provide the correct diagnosis preoperatively.5
Please cite this article as: Marchiori E, Zanetti G, Hochhegger B. Rol de las pruebas de imagen en las sospechas de tumor de arteria pulmonar. Arch Bronconeumol. 2016;52:222.