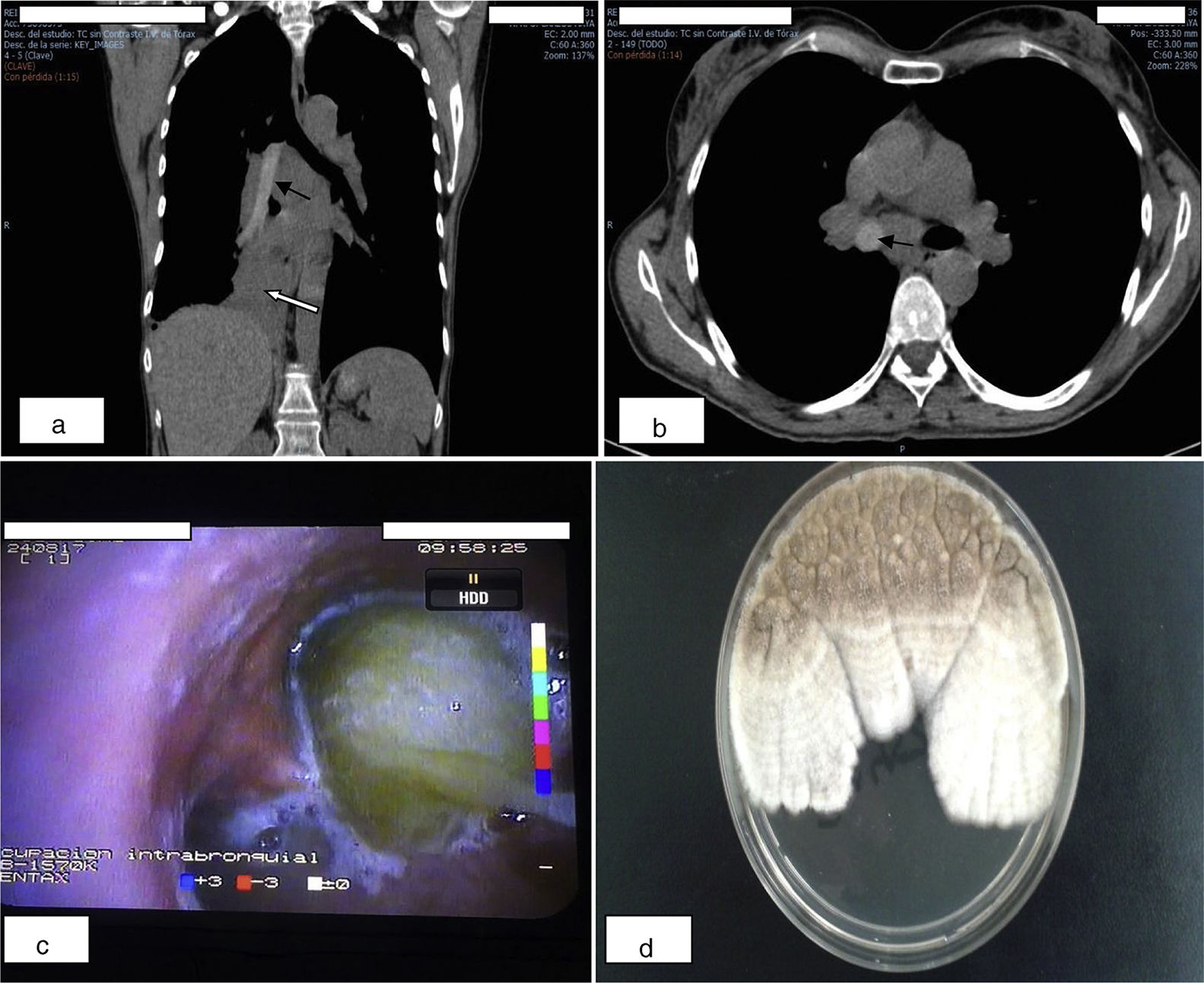
We report the case of a 52-year-old woman with a history of 3 episodes of pneumonia and asthma. She consulted due to dyspnea, chronic cough, and low-grade fever. Clinical laboratory tests showed eosinophilia 7.7% (0.5×109/l) and total immunoglobulin E (IgET): 6680IU/l. Skin prick and radioallergosorbent (RAST) tests were positive for Aspergillus. Computed tomography images are shown in Fig. 1a and b. Bronchoscopy (Fig. 1c) revealed a large, thick, purulent mucous plug in the entrance to the right pulmonary tree. Bronchial aspirate fluid showed fungal mycelia and Aspergillus terreus was isolated on culture (Fig. 1d). Cytology revealed inflammatory cells and fungal structures consistent with hyphae.
(a and b) Coronal and axial computed tomography images, showing high density material in the mediastinum (corresponding to the mucous plug) in almost all of the bronchial tree, with partial occupation starting at the entrance to the main bronchus, complete occupation of the intermediate bronchus, and complete occlusion of the lower and middle lobe bronchi (black arrows), causing partial atelectasis of the parenchyma dependent on these lobar bronchi (white arrow). Bilateral varicose bronchiectasis were also observed in the parenchymal images. (c) Bronchoscopic image of the mucous plug protruding from the entrance to the right bronchus just before aspiration. (d) Characteristic white, cottony Aspergillus terreus colonies isolated in Sabouraud chloramphenicol agar, that develop into cinnamon or coffee-colored powder or granules.
Allergic bronchopulmonary aspergillosis (ABPA) occurs in susceptible patients who are exposed to Aspergillus spores. ABPA affects severe asthmatics and, particularly, patients with cystic fibrosis. Diagnostic criteria do not always present simultaneously.1 In cases such as ours, in which asthma and bronchiectasis coexist, aspergillosis should be considered in the differential diagnosis.2 ABPA is currently subdivided into 2 different subgroups, with and without bronchiectasis. Criteria for ABPA-bronchiectasis are asthma, proximal bronchiectasis, raised IgET, positive skin test for Aspergillus spp, and raised specific IgE and/or IgG in serum.
Please cite this article as: Páez Codeso FM, Bermúdez Ruiz MP, Dorado Galindo A. Radiología, broncoscopia y microbiología de la aspergilosis bronco-pulmonar. Arch Bronconeumol. 2018;54:625.