Air leak syndrome (ALS) is a rare, severe, non-infectious complication of allogeneic bone marrow transplantation (ABMT) that generally affects patients with constrictive bronchiolitis (CB) in the context of graft-versus-host disease (GVHD). Prognosis is very poor.1–3 Diagnosis of ALS is usually radiological and it may present in the form of pneumothorax, pneumomediastinum, and interstitial and/or subcutaneous emphysema.4,5 We report a case of ALS 22 years after ABMT in a patient with a history of acute lymphoblastic leukemia.
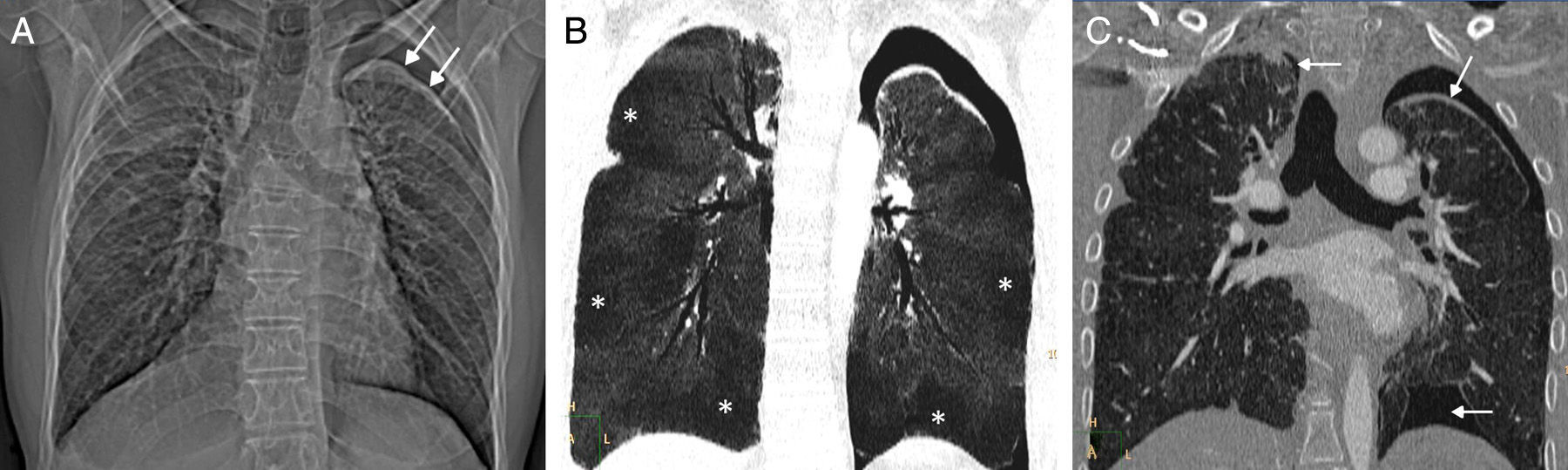
Our patient was a 32-year-old man who presented in our hospital with dyspnea on minimal exertion and chest pain. Significant history included acute lymphoblastic leukemia diagnosed at the age of 6 years, treated with chemotherapy and prophylactic cranial radiation therapy. Four years later, at the age of 10, he presented testicular relapse of the leukemia, and underwent ABMT after conditioning with chemotherapy and total body irradiation. The patient developed several non-infectious complications associated with his treatment regimen: primary hypogonadism, bilateral cataracts, growth hormone deficiency, syndrome of inappropriate antidiuretic hormone secretion, etc. At the age of 28 years (18 years after ABMT), the patient was diagnosed with CB in the context of grade I GVHD, in addition to skin and intestinal manifestations. He was treated with low-dose corticosteroids in an attempt to minimize the development of opportunistic infections, and because non-severe forms of GVHD have a “graft-versus-tumor” effect that reduces the likelihood of tumor relapse. However, the patient's lung function tests continued to deteriorate progressively despite escalation of the dose of corticosteroids. The patient also presented a first episode of left pneumothorax (4 months before admission to our hospital), which was treated with a chest tube in another center. At the time of admission to our hospital, he had a forced vital capacity of 1230ml (27.2% predicted) and a forced expiratory volume of 1060ml (27.7% predicted). Chest radiography revealed a loss of volume in both lungs and a new left pneumothorax (Fig. 1A). A chest computed tomography (CT) showed signs of CB with areas of air trapping (Fig. 1B) and bilateral pneumothorax (Fig. 1C), and a diagnosis of ALS was given. Despite placement of a left chest tube, the patient died 5 weeks later due to respiratory failure.
(A) Chest radiograph showing a loss of volume in both lungs and left pneumothorax (arrows). (B) Minimum intensity projection (minIP) coronal reconstruction of chest CT (pulmonary parenchyma window), showing geographical areas of low attenuation in both lungs (asterisks) associated with areas of air trapping. (C) Coronal image of chest CT (pulmonary parenchyma window) revealing bilateral pneumothorax (arrows).
ALS is a severe non-infectious complication of ABMT, consisting of extra-alveolar air in the chest in the form of pneumothorax, interstitial emphysema, pneumomediastinum and/or subcutaneous emphysema.1 This is a very rare complication, and practically all cases of ALS are associated with advanced CB in the context of chronic GVHD.2 However, in contrast to the generally slow clinical progress of CB (progressive dyspnea, tachypnea, cough), ALS can present in an acute form with chest pain and sudden onset of dyspnea. A diagnosis of ALS carries a very poor long-term prognosis for survival, so radiological detection has important therapeutic and prognostic implications.3 Most cases of ALS are diagnosed within a period of a few months to 6–7 years after ABMT, and the clinical suspicion of this process is generally confirmed on imaging tests (particularly chest CT). Although chest CT has become a very useful diagnostic tool in the diagnosis and follow-up of complications associated with ABMT, very few references in the literature describe radiological findings in ALS.4 Our case is interesting because we found no reports in the literature of such late onset of ALS after ABMT, and because only 3 previous cases of ALS with bilateral pneumothorax have been reported.5 We also believe that in patients who have undergone ABMT with a diagnosis (or clinical suspicion) of CB who present acute chest symptoms (chest pain and/or sudden dyspnea), a CT should be performed to rule out the various radiological manifestations of ALS.
Please cite this article as: Gorospe L, Cabañero-Sánchez A, Muñoz-Molina GM, Chinea-Rodríguez A. Neumotórax bilateral secundario a un síndrome de fuga aérea 22 años después de un trasplante alogénico de médula ósea. Arch Bronconeumol. 2017;53:459–460.