In the last 10 years, the treatment of lung cancer, especially non-small cell lung cancer (NSCLC) has changed following the development of new interventions targeting mutations detected in pathological samples of NSCLC.1 Some of the available molecular genes include epidermal growth factor receptor (EGFR), anaplastic lymphoma kinase (ALK), and ROS proto-oncogene 1 (ROS1), among others.2
Endobronchial ultrasound with transbronchial needle aspiration (EBUS-TBNA) is a minimally invasive technique with a high diagnostic yield, especially for central airway lesions. This technique is safe, and the European Respiratory Society (ERS), European Thoracic Society (ETS), European Society of Medical Oncology (ESMO), and American College of Chest Physician (ACCP) have suggested starting with this approach when diagnosing and staging lung cancer, especially NSCLC.3,4 The aim of this study is to identify the presence of 3 genetic alterations that can be targeted by specific therapeutic inhibitors, EGFR, ALK, and ROS1, collected by endobronchial ultrasound with transbronchial needle aspiration (EBUS-TBNA).
We performed a descriptive, prospective study of EBUS-TBNA samples between July 2014 and June 2015 in a reference center in Chile. Consent forms were signed by all patients and the protocol was approved by the ethics committee of our institution. The inclusion criteria were: (1) adult patients (>18 years old) with a lesion suggestive of lung cancer on clinical and radiological studies who underwent EBUS-TBNA (EBUS Olympus® and EBUS Fuji®) and (2) confirmed lung cancer by a pathological study (adenocarcinoma or not otherwise specified [NOS]). We performed mediastinal EBUS when CT scan showed lymphnodes greater than 10mm, or peripheral pulmonary lesions greater or equal to 30mm, or any central pulmonary lesions. Not all patients had undergone PET before EBUS was performed. We did not exclude patients with disseminated disease (EBUS performed for diagnosis purpose). Patients younger than 18 years, or who did not consent to the procedure were excluded. A minimum of 4 samples were obtained by EBUS-TBNA. Cell blocks were prepared from cytology samples and fixed with 10% formalin solution. All samples were covered with a paraffin solution followed by hematoxylin-eosin staining. Immunohistochemical staining, including TTF-1/napsin-A, CK 5/6 and p40 was performed in cases with no clear adenocarcinoma or squamous cell carcinoma morphology. Samples were subject to sequential molecular testing using the Sanger sequencing analysis (when tumor cell count was over 30%) or Cobas 4800 (needs less tumoral DNA, faster results, more expensive automatic technique) for EGFR mutation, depending on the volume of sample. In cases in which EGFR was negative, we proceeded to analyze the presence of ALK translocation using fluorescence in situ hybridization (FISH) (ZytoLight® SPEC ALK/EML4 TriCheck™ Probe). Finally, a third molecular test using FISH was performed for ROS1 (ZytoLight® SPEC ROS1 Dual Color Break Apart Probe). The primary objective was to determine if EBUS tissue samples were sufficient for molecular testing analysis. “Sufficient tissue sample”: we defined sufficient sample as the minimum concentration of a tumor marker achieved by EBUS-TBNA for which a mutation can be processed (a minimum mutated allele of 25% by Sanger method).
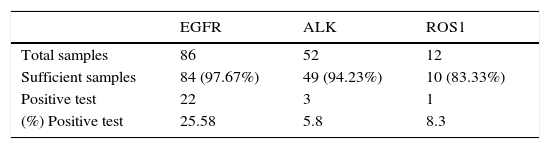
Eighty-six patients were included in this study, with 216 EBUS-TBNA performed. Forty-seven (54.65%) participants were female, and average age was 65.70 years (range 37–91). No complications were reported. Samples were obtained from lymphnodes in 60/86 (69.76%) patients and from lung parenchyma in 26/86 (30.24%) patients. Sufficient tissue sample was achieved in 97.67% (84/86) of samples for EGFR mutation, 94.23% (49/52 samples) for ALK translocation and 83.33% (10/12 samples) for ROS1 mutation.
Molecular testing was positive in 30.23% (26/86 samples), and the most frequent mutation was EGFR, which was present in 22/86 (25. 58%), followed by 1/12 cases for ROS1 (8.3%) and 3/52 cases for ALK (5.76%). A summary of results is shown in Table 1.
Genetic profile of EGFR demonstrated that deletion in exon 19 was the most frequent mutation (13 cases of delE746-A750 and 2 cases of del2235-2249), which was followed by an L858R amino acid substitution in exon 21 in 4 cases, and G719A amino acid substitution at position 719 in exon 18 was reported in 2 cases. Finally, exon 20 T790M acquired resistance mutation to tyrosine kinase inhibitors (TKIs) was identified in 1 patient.
This is the first report evaluating the efficacy of EBUS-TBNA for lung cancer and mutational testing in South America. Previous reports were performed in post-surgical samples.5
EBUS-TBNA is a safe method with a high diagnostic yield for lung cancer. In a randomized controlled trial, mediastinal staging by EBUS-TBNA was compared with standard techniques, consisting of imaging and surgical biopsy. The time to “confirmed” diagnosis was 2 weeks with this approach versus 4 weeks when using the conventional methods.6 In addition, the number of complications and economic analysis was lower in the EBUS-TBNA arm.
Several studies have evaluated the efficacy of EBUS-TBNA for molecular testing in lung cancer. In a multicenter study of 774 patients, EGFR analysis was possible in 90% of the patients analyzed.7,8 This is consistent with the prevalence described in our series.
In a recent study by Casadio et al., EBUS-TBNA was performed in 306 consecutive patients with stage IIIB-IV lung cancer by TNM. EGFR analyses were performed in 195 patients, and a cytological diagnosis was achieved in 95.1%. EGFR mutations were present in 16.9%, ALK in 3.9% and KRAS in 31.6%. In addition, chi-square analysis to compare the percentage of mutations in a historical surgical series found no differences.9 This is consistent with the prevalence described in our series.9
The genetic profile is similar to that reported by other South American countries. De Melo et al., reported the mutational profile for 125 patients with lung adenocarcinoma, and EGFR mutations were found in 21.6%, ALK in 4.8% and KRAS in 26.4%.5 Our study is one of the few to have reported the utility of EBUS-TBNA for identifying ROS1 mutation, and resistance mutation to TKIs.
This study has limitations. We did not compare our negative EBUS results with surgery or response to target molecular therapy. In our center, we perform an average of 220 EBUS-TBNA procedures per year, with diagnosis of lung adenocarcinoma in approximately 70% of cases. Since we are a regional reference center for EBUS-TBNA, some patients are lost to follow-up and complete their sample processing in the referral center. This is why the number of patients who underwent mutational testing was low. The number of samples for ROS1 testing was limited, thus a study with more cases is required for further analysis.
In conclusion, EBUS-TBNA is a useful minimally invasive technique for collecting cytopathological samples and performing molecular mutation analysis in our lung cancer patients. Samples can also be used to evaluate acquired resistance mutation.
Please cite this article as: Fernandez-Bussy S, Labarca G, Pires Y, Caviedes I, Burotto M. Análisis moleculares de EGFR, mutación de resistencia al EGFR, ALK y ROS1 en muestras obtenidas mediante PATB-USEB en Chile. Arch Bronconeumol. 2017;53:172–174.