Congenital lung malformations (CLM) are a group of entities caused by alterations in the embryogenesis of the lung and airways. Both the site within the tracheobronchial tree and the gestational age at the time of the embryological insult correlate with lesion type and histopathology.1
Clinical, radiological and histopathological criteria have been established for the classification of most CLM. Diseases currently considered CLM are congenital pulmonary airway malformations (CPAM), pulmonary sequestration, bronchogenic cyst, congenital lobar emphysema, and bronchial atresia. Stocker2 classifies CPAM, formerly known as congenital cystic adenomatoid malformation, into 5 subtypes based on the number and size of the cysts and their anatomical origin: Type 0: lung consisting of small cysts (0.5cm), incompatible with life; Type 1: single or multiple cysts (2–10cm), arising from the bronchi or bronchioles; Type 2: multiple cysts (0.5–2cm) in the bronchioles; Type 3: solid lesion with cysts (<0.5cm) in the bronchioles and alveolar tract; and Type 4: cysts up to 7cm, originating in the distal acinar region.
Pulmonary sequestration refers to a non-functioning sector of the lung that is irrigated by the systemic circulation, and is classified as intralobar or extralobar, depending on whether it is contained within the visceral pleura of lung or it has its own pleural lining, respectively.1
CLMs are rare, accounting for between 7.5% and 18.7% of all organ malformation, and their clinical presentation and severity vary widely, especially in terms of the degree of pulmonary involvement. Manifestations can occur at any age, but typically develop in infancy and childhood. The risk of recurrent respiratory infections or malignant transformation has been described in the course of some CLM, particularly CPAM.3,4
CLM may be diagnosed at birth due to the onset of clinical symptoms, incidentally during radiological studies, with or without symptoms, or in ultrasonography tests performed in the prenatal period.1,4,5
The management of these lesions depends on the type of malformation and the development of symptoms, so management must be individualized for each case and type of malformation; most authors recommend resection of the lesion, but there is currently no consensus on the surgical approach, especially in asymptomatic patients.3,6,7
The aim of this review is to describe the clinical, radiological, pathological findings, progress, and follow-up of 20 children diagnosed with CLM in the University Hospital Parc Taulí between 2006 and 2016.
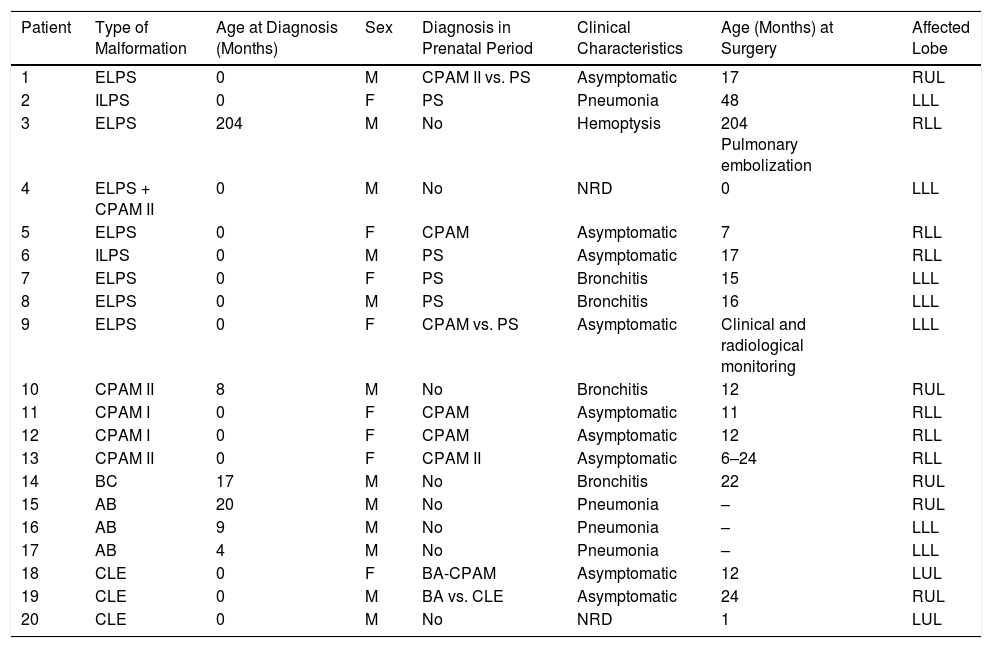
We reviewed the medical records of 20 children with CLM: 12 boys (60%) and 8 girls (40%). Twelve children (60%) were diagnosed during the prenatal period. Congenital lung malformations were identified as: pulmonary sequestration: 9 cases, (45%), 7 extralobar (77.7%), 2 intralobar (22.22%); CPAM: 5 cases (25%), subtype I: 3 (60%), subtype II: 2 (40%), 1 associated with extralobar sequestration; bronchial atresia: 3 (15%); bronchogenic cyst: 1 (5%); congenital lobar emphysema 3 (15%). Clinical presentation in the postnatal period was as follows: 2 patients had neonatal respiratory distress; 9 patients (45%) were asymptomatic; 3 (15%) had recurrent lung infections; and 6 (30%) had episodes of bronchitis. Diagnostic fiberoptic bronchoscopy was performed in the 3 cases of bronchial atresia and lesion sites were distributed as follows: 5 in RUL, 7 in LLL, 6 in RLL, and 2 in LUL. Sixteen were treated with surgery (80%) at an average age of 14 months (2 days-48 months) (Table 1).
Patient Characteristics.
| Patient | Type of Malformation | Age at Diagnosis (Months) | Sex | Diagnosis in Prenatal Period | Clinical Characteristics | Age (Months) at Surgery | Affected Lobe |
|---|---|---|---|---|---|---|---|
| 1 | ELPS | 0 | M | CPAM II vs. PS | Asymptomatic | 17 | RUL |
| 2 | ILPS | 0 | F | PS | Pneumonia | 48 | LLL |
| 3 | ELPS | 204 | M | No | Hemoptysis | 204 Pulmonary embolization | RLL |
| 4 | ELPS + CPAM II | 0 | M | No | NRD | 0 | LLL |
| 5 | ELPS | 0 | F | CPAM | Asymptomatic | 7 | RLL |
| 6 | ILPS | 0 | M | PS | Asymptomatic | 17 | RLL |
| 7 | ELPS | 0 | F | PS | Bronchitis | 15 | LLL |
| 8 | ELPS | 0 | M | PS | Bronchitis | 16 | LLL |
| 9 | ELPS | 0 | F | CPAM vs. PS | Asymptomatic | Clinical and radiological monitoring | LLL |
| 10 | CPAM II | 8 | M | No | Bronchitis | 12 | RUL |
| 11 | CPAM I | 0 | F | CPAM | Asymptomatic | 11 | RLL |
| 12 | CPAM I | 0 | F | CPAM | Asymptomatic | 12 | RLL |
| 13 | CPAM II | 0 | F | CPAM II | Asymptomatic | 6–24 | RLL |
| 14 | BC | 17 | M | No | Bronchitis | 22 | RUL |
| 15 | AB | 20 | M | No | Pneumonia | – | RUL |
| 16 | AB | 9 | M | No | Pneumonia | – | LLL |
| 17 | AB | 4 | M | No | Pneumonia | – | LLL |
| 18 | CLE | 0 | F | BA-CPAM | Asymptomatic | 12 | LUL |
| 19 | CLE | 0 | M | BA vs. CLE | Asymptomatic | 24 | RUL |
| 20 | CLE | 0 | M | No | NRD | 1 | LUL |
BA: bronchial atresia; BC: bronchogenic cyst; CLE: congenital lobar emphysema; CPAM: congenital airway lung malformation; ELPS: extralobar pulmonary sequestration; ELPS: intralobar pulmonary sequestration; LLL: left lower lobe; LLL: left upper lobe; NRD: neonatal respiratory distress; PS: pulmonary sequestration; RLL: right lower lobe; RUL: right upper lobe.
In the group of 9 asymptomatic patients (45%), 8 were treated with surgery, and of these 2 had congenital lobar emphysema, 3 CPAM, and 3 pulmonary sequestration. One patient with CPAM type II required 2 surgical interventions (6 and 24 months of age), with subsequent clinical and radiological follow-up, in view of persistent CPAM. The asymptomatic patient who was not treated with surgery was a case of extralobar pulmonary sequestration that was managed conservatively with a favorable outcome.
The most common lung malformations in our series were CPAM and pulmonary sequestration. Prenatal ultrasonography provided the diagnosis in more than half of the cases. The chest X-ray of most patients diagnosed by prenatal ultrasonography was normal in the neonatal period, and diagnosis was confirmed in all patients with chest CT. Eighty percent of the children were treated with surgery, with no postoperative complications. The remaining patients continued to progress favorably in the 10 years of follow-up.
As reported in other reviews, the diagnosis of this disease has increased with the use of prenatal ultrasound, while chest CT remains the gold standard diagnostic method. According to the literature, the management of asymptomatic patients is still controversial, and many authors are inclined toward early elective surgery to avoid the risk of complications including infections and the risk of malignant transformation.8,9 In our review, about half the patients were asymptomatic, and most were treated with surgical resection.
Criteria for surgery have been identified in patients at higher risk, while conservative management may be selected for lower-risk patients.3,10 Proponents of non-surgical treatment report that some CLM can spontaneously resolve in the postnatal period, but the prevalence of complications is unknown.6
The current trend is toward performing minimally invasive pulmonary resections via video-assisted thoracoscopy, due to the low morbidity and good postoperative results offered by this procedure.11,12
The involvement of a multidisciplinary team is of vital importance in the management of these patients, and the most appropriate treatment should be selected according to the type of malformation and the presence of symptoms, taking into consideration the risk of complications in each case and the benefit of surgery.
Please cite this article as: Lovera de Ferreira CT, Serra Azuara L, Asensio de la Cruz O, Bosque García MM. Malformaciones congénitas pulmonares diagnosticadas en un periodo de 10 años. Arch Bronconeumol. 2018;54:165–167.