Currently, the most widely accepted opinion is that allergic mechanisms play a decisive role in the pathogenesis of most types of asthma. Animal models that are used for researching the mechanisms that intervene in the disease are largely based on this assumption. In fact, it has been known for some time that asthma is associated with an increase in serum levels of immunoglobulin E (IgE), a specific type of antibodies that, in addition to being involved in the immune response of mammals compared with parasites, also play an important role in allergic hypersensitivity. One of the most notable elements of evidence that support the association between IgE and asthma comes from the Tucson Epidemiological Study of Airway Obstructive Disease (TESAOD) study, in which Burrows et al. demonstrated an almost linear relationship between increasing IgE serum levels and the risk for asthma in the general population.1
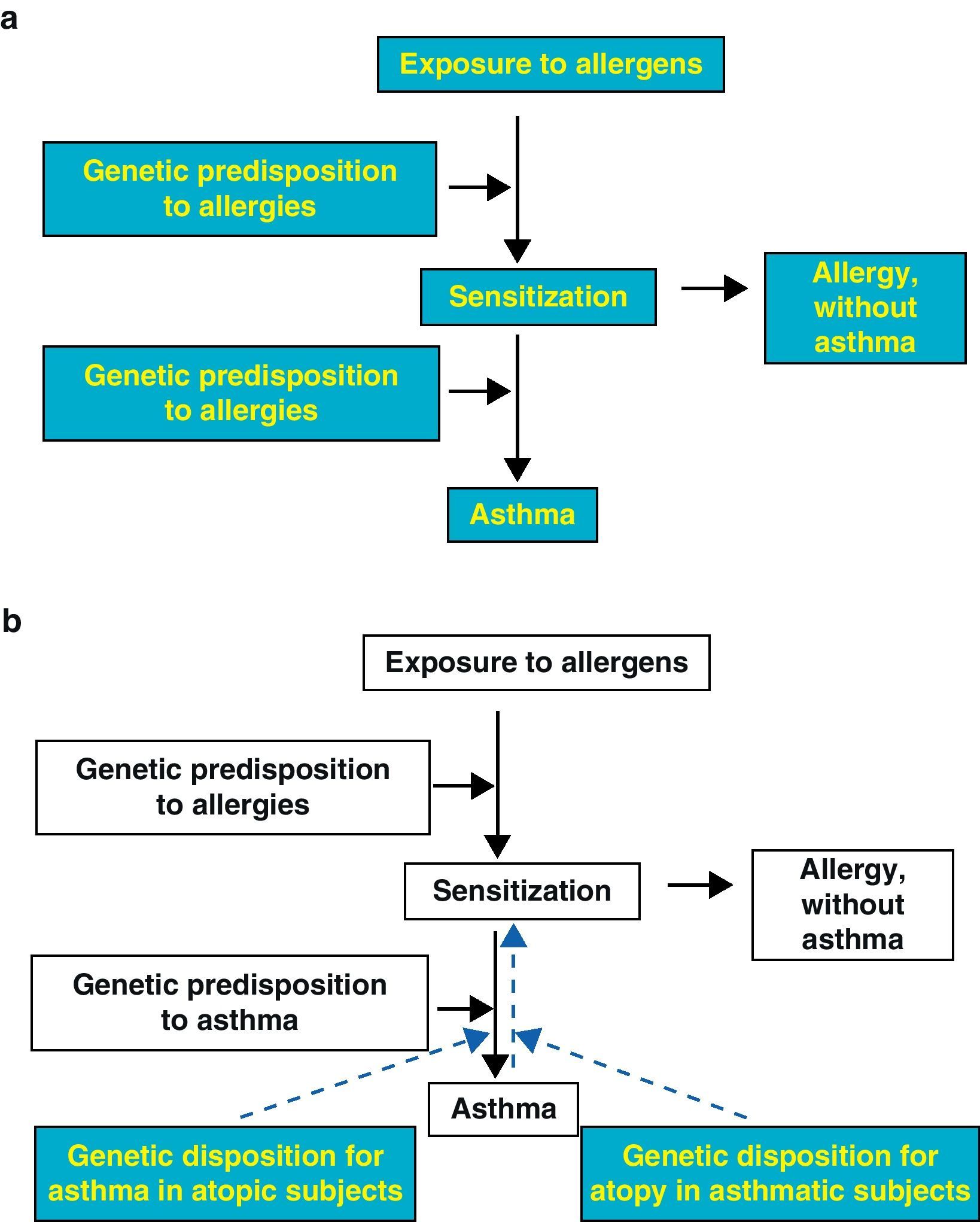
The relationship of serum IgE and the phenotype closely related with it for cutaneous allergic sensitization with asthma has been traditionally interpreted as a two-stage unidirectional causal model (Fig. 1a), in which the exposure to allergens would lead to allergic sensitization and this, at the same time, to increased risk for asthma. In this causal pathway, genetic susceptibility would play an important role in determining which exposed individuals would develop sensitization and which sensitized individuals would wind up developing asthma. Consequently, if this model were correct, it would be predictable that an important part of the hereditary nature of asthma would be explained by genetic determinants for IgE levels, and that a considerable number of genetic variants that affect the risk for asthma would also be associated with allergic sensitization and high serum IgE. It should be highlighted that neither of these two hypotheses have turned out to be correct. In the Tucson Children's Respiratory Study, for instance, the results of the segregation analysis of asthma confirmed by a physician in almost 3400 individuals from 906 family nuclei remained unaltered when IgE was added to the models as a covariable.2 Furthermore, in the largest whole genome association study ever done in asthma that was recently completed,3 very little overlapping was observed among the polymorphic loci that confer the susceptibility to asthma and those that control serum IgE levels. These observations suggest that the increased IgE could be an epiphenomenon rather than a cause of asthma.
In this context, we suggest that most of the epidemiological and experimental evidence that has been accumulating about this topic in the last two decades clearly indicate a much more complicated inter-relationship between asthma, allergic sensitization and serum IgE than what is proposed by a simple unidirectional causal model. In the first place, although the majority of the epidemiological studies have shown that the level of exposure to domestic allergens in the initial phase of life correlates positively with the risk for allergic sensitization and that, at the same time, allergic sensitization to domestic allergens significantly increases the risk of phenotypes related with asthma (such as wheezing) during childhood, several studies have not been able to identify a direct relationship between early exposure to allergens and asthma. In one, the German Multicentre Allergy Study,4 the children who were in the highest quartile for exposure to house dust mites at the age of 6 months showed a significantly higher probability for sensitization to mites at the age of 5 when compared with those in the lowest quartile. However, at no time during the follow-up between the ages of 1 and 7, there was a difference observed between the low allergen exposure group and the high allergen exposure group regarding the current prevalence of wheezing or diagnosis of asthma.
It should be emphasized that these apparently surprising data from observational studies have been confirmed in several experimental assays. Among these is the Childhood Asthma Prevention Study,5 in which researchers evaluated the effects of an intervention for avoiding house dust mites that included using impermeable mattress protectors and an acaricide in small children. When compared with the control group, even though the intervention group showed a reduction of up to 75% in the concentrations of house dust mite allergens in the dust samples obtained from the child's bed at the age of 1, the intervention was observed to have no effect at all on the prevalence of wheezing or asthma either at the age of 1 or later up until the age of 5, as confirmed by a doctor in the 616 participating children.6 Thus, in a randomized intervention assay, the avoidance of exposure to allergens did not reduce the risk for asthma, which brings into doubt the fundamental evidence considered for establishing a causal relationship between exposure and clinical results.
In addition to the mentioned observations, the causal character of the relationship between IgE and asthma has also been brought into doubt by the results of family-based cohort studies. For example, in another TESAOD study,7 although it was observed that high IgE levels in the parents was an independent risk factor for asthma in their children, the children with asthma presented considerably higher serum IgE levels than what could be expected according to the parental IgE levels. In other words, the presence of asthma seemed to increase the IgE of the children above what would be expected according to their genetic predisposition alone. Based on these data, the authors proposed for the first time the hypothesis that the inflammation of the respiratory tract associated with asthma could alone increase serum IgE levels, possibly through cytokines and other immune mediators that are generated in the airways by the processes of the disease.
Ten years later, the implications of these results were extended by what was observed in another longitudinal cohort study: the Tucson Children's Respiratory Study.8 They divided the children of this cohort from birth into four groups depending on the results obtained with the combination of the skin tests for sensitization and the presence of asthma in the parents. As was expected, the children of atopic parents had a greater probability of presenting positive skin tests when compared with the children of non-atopic parents. However, one more surprising observation was that, among the children of atopic parents, those that had at least one parent with asthma showed a significantly higher probability of having positive skin tests than the children with non-asthmatic parents. This suggests that the predisposition for asthma independently increased the risk for atopic sensitization. This effect could not be simply attributed to a “more intense” allergy phenotype in atopic parents with asthma in comparison with atopic parents without asthma, as it was independent of the characteristics of the parental atopy, including the number of positive skin tests, maximum bump size, serum IgE values and the number of atopic progenitors. After adjusting for these characteristics of parental atopy, the fact that at least one of the parents was asthmatic continued to increase the probabilities that the child would develop atopy by 50%.
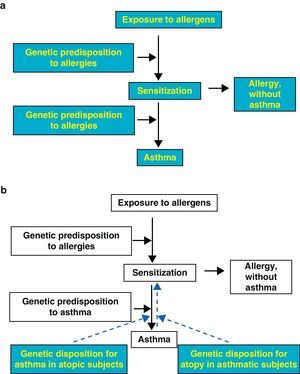
Considered together, the observations made in the cited studies provide solid evidence for a theoretical model in which the arrow that indicates the connection between atopic sensitization and asthma can go, at least partially, backwards, meaning from asthma to sensitization (Fig. 1b). In this bidirectional model, it seems plausible that there are different genes that influence each of the two components of the arrow in “sensitization↔asthma”, and this scenario is compatible with the limited overlapping of the polymorphic loci that affect both phenotypes, as has been observed in previous family association and aggregation studies.
The mechanisms by which asthma can increase the susceptibility to atopy have not yet been clarified. Nevertheless, it is possible that the epithelial lesion and the inflammation associated with it in the airways of asthmatic patients can play an important role in the promotion of atopic sensitization and the production of IgE. In recent years, there have been new analyses on the possible roles of activation of the epithelium in the airways and the associated promotion of the local synthesis of cytokines, chemokines and growth factors to create the micro-environment necessary for the polarization of Th2 and the later production of IgE.9 In this scenario, the epithelial lesion of the airways associated with asthma can set in motion mechanisms that lead to allergic sensitization, which (after repeated exposure to the allergens) can at the same time promote and prolong the inflammatory response of the airways and cause a persistent disease with a spiral of positive feedback.
In conclusion, there is extensive epidemiologic, clinical and experimental evidence that raise doubts about the unidirectional model that has been traditionally used for interpreting the association between atopy and asthma, in which the exposure to allergens leads to allergic sensitization, which in turn causes asthma. Instead, we propose that the association between atopy and asthma concurs, at least in part, with an alternative model where the development of asthma and the epithelial anomalies associated with it predispose the airways to a local sensitization that, once established, would have the effect of aggravating the inflammatory response and remodeling. In this context, we propose that understanding the nature and the direction of the relationship between IgE and asthma will have crucial implications for the prevention and treatment of this disease. This, at the very least, may raise doubt about the degree at which prediction models and pharmacological interventions should be directed by serum IgE, which continues to be the asthma marker that is first identified even though our understanding of it is still limited.
Please cite this article as: Guerra S, Martinez FD. ¿Es la alergia una enfermedad asmática? Arch Bronconeumol. 2011;47:479-81.