Classifying pleural effusions into transudates and exudates is the first step in the diagnostic study of pleural fluid.1 Some authors have suggested that instilling 30% hydrogen peroxide (H2O2) drops in the pleural fluid sample could help in this classification, providing information at the bedside at the time of thoracentesis.2,3 H2O2 is a strongly oxidizing chemical compound that decomposes in a very exothermic reaction into water and oxygen, producing visible bubbles. The high catalase activity of exudates would accelerate the decomposition of H2O2, leading to the appearance of bubbles.2 However, this possibility has not been evaluated in adequate patient samples; moreover, at a concentration of 30%, H2O2 is toxic.4
This study aimed to assess a commercial formulation of H2O2 3% for differentiating pleural transudates and exudates at the bedside. We designed a prospective study, including consecutive patients with pleural effusion who underwent diagnostic thoracentesis. Only the result of the first thoracentesis was considered, and cases with more than one alternative diagnosis, empyema and the hemothorax were excluded. The following data were collected for each case: age, sex, appearance of the pleural fluid, and red blood cells. The pleural fluid was studied according to the usual methods. Immediately after pleural fluid extraction, 1mL of H2O2 3% was added to a 2mL aliquot of pleural fluid in a 150mm×10.2mm test tube (volume 23mL). After shaking the sample lightly for 10s, the tube was visually inspected for bubbling, and the volume of gas produced after 1min, 3min, and 5min was measured using a ruler with millimeter measurement (Fig. 1). The Mann–Whitney U test was used to compare the results. and the area under the receiver-operating characteristics (ROC) curve was determined to analyze diagnostic accuracy. p values of less than 0.05 were considered significant. The study was approved by the Clinical Research Ethics Committee of the Elche General University Hospital (PI 74/2022), and all included patients gave their informed consent.
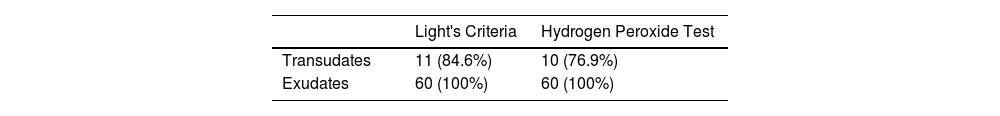
In the present study, 81 cases were included during a period of one year. Of these, 8 were excluded. In total, 73 patients (38 women, 52%) with a mean age of 67 years (standard deviation [SD] 15) were included. The effusions comprised 13 (18%) transudates (8 heart failure) and 60 (82%) exudates. Regarding etiology, the effusions in the exudates group were secondary to malignant disease in 31 (52%) cases, infectious origin in 16 (27%), and due to other benign processes in 13 (21%). There were no effusions of tuberculous origin. Gas formation was observed after H2O2 instillation in 63 (86.3%) samples. The most applicable value was at 3min and, to classify exudates, the AUC at 3rd min was 0.84. The median gas volume produced at 3min was 2mm (interquartile range [IQR] 0–16) in transudates and 32.50mm (IQR 16.25–50.75) in exudates (p=0.001). Table 1 shows the effusions correctly classified by Light's criteria and by the hydrogen peroxide test at 3rd min. The sensitivity of both tests for classifying exudates was 100% and the specificity and specificity were 76.9% for H2O2 and 84.6% for Light's criteria.
In the three transudates where gas formation was observed, the appearance of the liquid was serohematic in two, and the third had an orange tinge. Analysis showed that all three contained a high number of red blood cells. Regarding the characteristics of the transudates misclassified by the hydrogen peroxide test, one of the effusions with a serohematic appearance was due to a traumatic puncture in a patient with heart failure; the red blood cell count was 147,200/mm3. The other serohematic effusion was obtained in a patient with hepatic hydrothorax and coagulopathy, the red blood cell count was 49,600/mm3. The third case, with an orange appearance, corresponded to a patient with heart failure, the red blood cell count was 4260/mm3 and the sample was slightly stained with blood during the puncture. However, the median number of red blood cells in non-hematic transudates was 325/mm3 (range 10–2720). Thus, H2O2 correctly classified all non-hematic transudates. Two of the transudates that did not show bubble formation was misclassified by Light's criteria as exudate. One of them was receiving diuretic treatment for heart failure and did not present gas bubble formation with H2O2.
In the study of pleural fluid, the determination of biochemical parameters is the first step to differentiate transudates from exudates.5,6 The criteria proposed by Light1 have some limitations, especially if the patient is receiving diuretics,7 but they continue to be the most accurate and widely used. However, a serum sample is necessary to calculate the results, and these are not obtained immediately, so an alternative technique to classify transudates and exudates could be of great clinical utility. Our study differed from previous ones2,3,8 by rigorously assessing a commercially available, low-concentration formulation of H2O2. The H2O2 test is simple, inexpensive, and safe for both the patient and the examiner. It can be performed at bedside immediately after thoracentesis. Sakar et al. studied the reaction after adding H2O2 30% to pleural fluid. The authors found differences between transudates and exudates, suggesting that the test could be a good rapid screening method. However, they excluded effusions with a hematic appearance, and the patients studied were not consecutively included.2 Subsequently, Taksande et al. used high concentrations of H2O2, reporting sensitivity of 80.7% and specificity of 81.8%3; however, their results are based on visual observation of bubbles, with no quantification of the volume of gas produced by the reaction, and they did not meet Light's criteria. Likewise, the authors did not establish cutoff values for the differentiation of pleural effusions.3,8
Although our results do not improve Light's criteria either, we obtained a high yield in the differentiation of effusions with the use of commercial presentation at low concentrations of H2O2. Exudates, by presenting greater catalase activity, accelerate the decomposition of H2O2 into acute and oxygen, producing the formation of visible bubbles.2
Additionally, since we did not exclude serohematic fluids, our research provides real-world data from routine clinical practice, demonstrating for the first time, that the addition of 1mL of H2O2 3% to pleural fluid can help immediately differentiate transudates and exudates in non-hematic effusions. It is known that the presence of red blood cells increases the catalase activity of the effusions and therefore the formation of gas bubbles when hydrogen peroxide is added.2 Therefore, in our experience, if there is no bubble formation after the application of the H2O2 3%, no additional (and sometimes invasive) studies would be necessary since it is a pleural transudate. Thus, we believe that the main advantage would be the correct classification of transudative effusions, when a clear-looking liquid is obtained and no reaction occurs when adding hydrogen peroxide. In these cases, it can support the initial clinical impression, and avoid additional diagnostic studies. For example, this test could be useful in cases with pleural effusion due to heart failure and diuretic treatment that can be erroneously classified as exudates by Light's criteria, as we observed in one of the cases in our series, no gas bubbles were formed. To validate our results, it would be necessary a future multicenter study that included non-hematic pleural effusions.
Despite the limitations of our study, including its single-center setting and small sample, our results show that the rapid hydrogen peroxide 3% test is a fast, simple, harmless and efficient way to differentiate exudates and non-hematic transudates at the patient's bedside.
Conflicts of InterestThe authors declare they have no conflict of interests.