Exacerbations are significant events in the natural history of chronic obstructive pulmonary disease (COPD) that can negatively impact patient quality of life, cause loss of lung function, limit survival, and foster the appearance of cardiovascular events.1–3 Approximately 30% of these episodes require evaluation by emergency services or even hospital admission, exerting severe pressure on healthcare systems.3 The weeks following an exacerbation of COPD (ECOPD) are crucial due to the high risk of recurrence, while in the 3 months after hospital discharge after ECOPD, the estimated mortality rate is around 11% and up to 40% of patients require readmission.3–5
Patients with chronic respiratory failure and frequent previous exacerbations who are older or have several comorbidities (especially cardiovascular conditions) are more predisposed to unfavourable outcomes.4 Therefore, when treating an exacerbation, interventions designed to both hasten resolution and prevent new events are essential. Indeed, prevention is one of the most important challenges in the care and management of this disease,1–5 demanding adequate continuity of care, the coordination and synchronisation of all actions and interventions, the optimisation of available resources, regardless of where they are delivered, and the prioritisation of actions that enable patients to return to baseline quickly and safely.3,6–8 Such interventions could allow early detection of ECOPD events, enable the correction of treatment errors, and improve patient self-care.1–3
Although the evidence is scarce, it seems that in up to half of ECOPD cases, no formal mechanisms are in place to guarantee adequate patient follow-up, even in hospital settings,5,9 and it may be difficult to achieve these goals. This is an important current and future challenge facing our health systems. Given the volume of cases, their seasonality, and varying levels of complexity and severity, the care and management of patients in the weeks following ECOPD should be shared between general primary care (PC) practitioners, pulmonology departments, and other medical specialisms. However, we are still encountering important communication and coordination barriers between these different levels of care.6,7 Some experts have stated that adequate protocolised and coordinated follow-ups by PC and hospital departments after ECOPD constitute the basic pillars of the integrated model of care for chronic COPD patients.8
No specific scheme or model has yet been identified as optimal for treating this disease, and those already in place are heterogeneous and do not adequately respond to the disease complexities of individual patients or the realities of the healthcare available within different health services. In Spain, some autonomous communities use institutional guidelines to guarantee continuity of care at this critical time, but no data have been published on the outcomes of these projects.6,7 In this respect, numerous multidimensional barriers and limitations to the follow-up of ECOPD have been described to date, citing factors related to both the organisation of health systems and healthcare professionals and patients themselves.7,8
Clinical guidelines and documents prepared by experts1–3 have specifically addressed care coordination and transition, but much of this work has been somewhat superficial, with recommendations limited to a series of scheduled appointments and general actions (‘discharge care bundles’) that often do not account for the potential complexity and vulnerabilities of each specific case.7,8 The professionals responsible for ECOPD care are often not fully aware of this key information; they rarely have access to adequate stratified records or certain complementary tests or treatments, and no specific alert systems are in place.7,8 Thus, the care provided to patients after ECOPD is often more reactive than preventive. A combination of preventive and reactive medicine, with scheduled appointments interspersed with case management, is desirable, but proactive follow-up and care on demand is currently difficult to achieve within the Spanish healthcare system, except in the case of certain special programmes that have been implemented in a limited number of centres.10
The transfer of information between professionals and patients is another essential factor in providing adequate continuity of care. Moreover, in the digital era, optimising the appropriate use of electronic medical records to improve communication between professionals and patients will be important. Telemedicine also offers a myriad of potentially useful tools in certain contexts, with the caveat that such solutions are not comprehensive and must be validated and optimised in each specific health area.11,12 Although the evidence for the use of telematic tools after hospitalisation for COPD seems to be generally favourable,12 we should underline the wide variability between the various studies and experiences reported, and the fact that results were sometimes contradictory, even when very similar models were applied. This heterogeneity makes it very difficult to generalise these results, since much of the previously published work was highly dependent on the specific infrastructures, information and communication technologies, and healthcare personnel available to the authors at the time.
The effect on outcomes of telemonitoring or home monitoring programmes, especially those based on patient education and self-monitoring interventions normally included in such programmes, is equally difficult to define.11,12 Elements that can hinder adequate continuity of care after ECOPD and must be considered in individualised programmes if positive results are to be achieved include patient knowledge of COPD, access to and competence in the use of digital technologies, and the specific needs, values and expectations of patients and their loved ones.7,13 Another factor that is becoming increasingly important in the continuity of care after ECOPD is the availability of the healthcare professionals needed to execute and coordinate all the recommended activities, especially since the frequency of these episodes tends to progressively increase over time, spiking in certain months of the year. This creates an overload in the burden of care and a shortfall in allotted resources for which contingency plans are generally unable to compensate.7,14
Apart from some specific experiences in certain patient collectives, few validated continuity of care schemes or models have been implemented in the Spanish healthcare landscape to significantly overcome the above-mentioned barriers and consistently and comprehensively minimise the health, social, and economic impacts of ECOPD complications.7
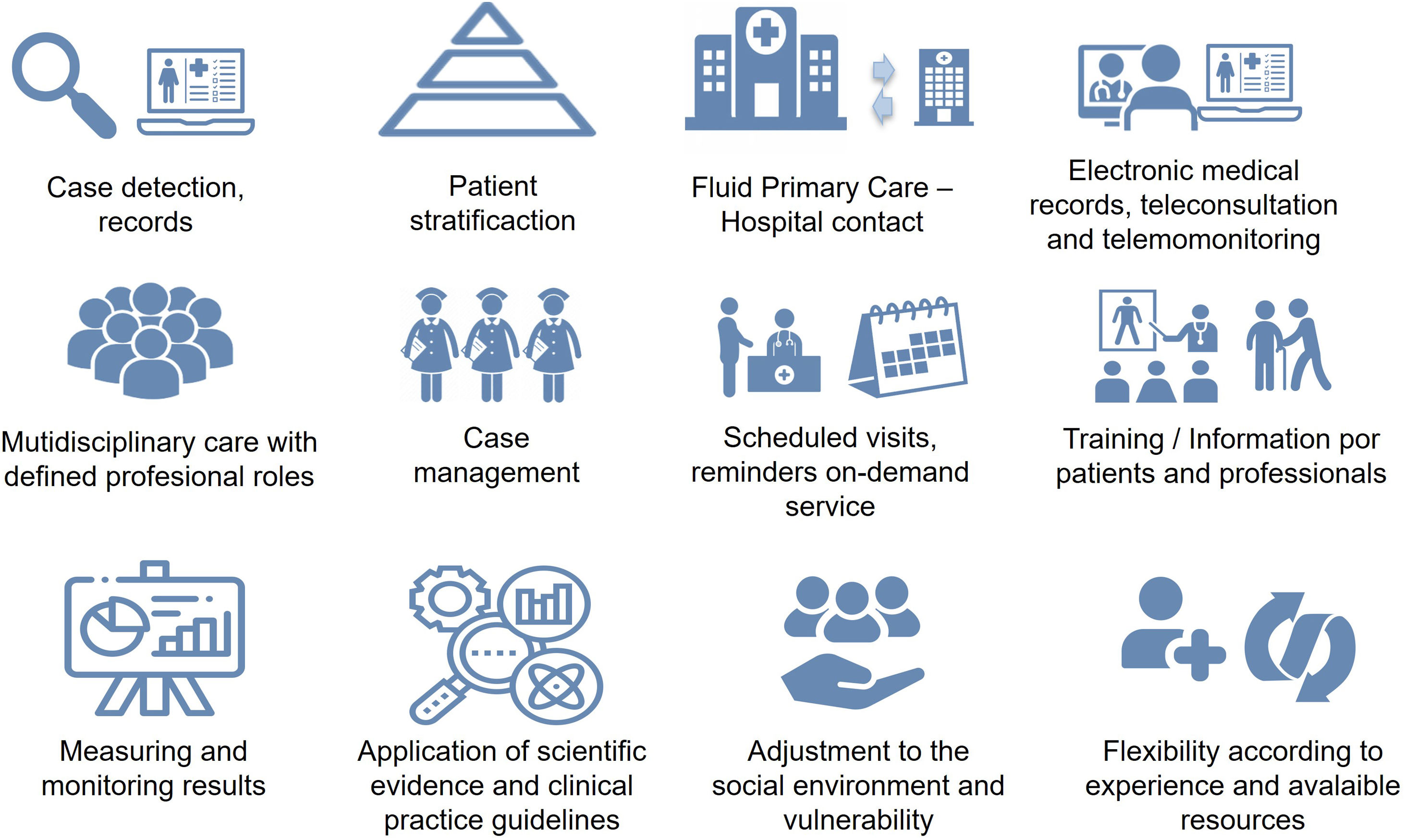
The ‘Referral Criteria in COPD and Continuity of Care’ document, recently published by SEPAR and other scientific societies including SEMERGEN, semFYC, SEMG, SEFAC, and GRAP, proposes a series of key elements to help develop continuity of care programmes (Fig. 1) that could be especially relevant in patients with ECOPD.15 This publication could serve as a theoretical framework for the development of adequate care schemes for these patients. Importantly, any such intervention programmes must be appropriately sized and be agreed upon by both patients and the various healthcare stakeholders. Their results must also be audited periodically so that they can be appropriately adapted to the realities of each specific health area.3,7,15
Key elements for adequate continuity of care in COPD.
No artificial intelligence tool has been used to prepare this manuscript.
FundingThis research has received no specific support from public sector agencies, the commercial sector or non-profit organisations.
Conflict of interestAFV has received honoraria for teaching activities or research grants from the following companies: AstraZeneca, Bial, Boehringer, Chiesi and GlaxoSmithKline.
JEC has received honoraria in the last three years for spirometry and COPD courses from semFYC and SESPA.
JMFG has received honoraria for speaking engagements and funding for conference attendance from Laboratories Esteve, MundiPharma, AstraZeneca, Boehringer Ingelheim, Ferrer, Menarini, Rovi, GlaxoSmithKline, Chiesi, Novartis, and Gebro Pharma.
JMD has received honoraria and funding from Laboratories AstraZeneca, Bial, Boehringer, Chiesi, Esteve, FAES, Ferrer, Gebro Pharma, GlaxoSmithKline, Janssen, Menarini, MundiPharma, Novartis, Roche, Rovi, Teva, and Pfizer.